A newly presented study at the ENDO 2025 meeting offers clinically significant insights into the impact of GLP-1 receptor agonist interruptions on weight loss outcomes. As global demand for medications such as semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) continues to rise, many patients face interrupted access due to supply shortages, insurance issues, or cost constraints.
This study, conducted by researchers at Calibrate, a commercial metabolic health program, reveals that substantial weight loss can still be achieved despite medication gaps, highlighting the potential resilience of integrated care approaches that combine pharmacologic and behavioral interventions.
Keywords: GLP-1 receptor agonists, Ozempic discontinuation, weight loss, semaglutide, tirzepatide, treatment gaps, ENDO 2025
Background
GLP-1 receptor agonists have become a cornerstone in the management of obesity and type 2 diabetes, providing significant benefits in appetite suppression, delayed gastric emptying, and glycemic control. Their weight loss efficacy has been well established in randomized controlled trials. However, limited access — whether due to cost, insurance coverage, or drug shortages — raises concerns about treatment continuity and its impact on long-term outcomes.
The current study was designed to assess real-world weight loss trajectories among individuals who experienced interruptions in GLP-1 therapy.
Methods
Researchers analyzed data from 6,392 adults enrolled in Calibrate’s commercial metabolic health program. Eligibility required that participants had:
- Received ≥1 month of GLP-1 receptor agonist treatment, and
- Completed ≥12 months in the program, which included personalized lifestyle coaching focused on nutrition, physical activity, sleep, and emotional well-being.
A treatment interruption was defined as a period of 13 weeks or more without GLP-1 therapy.
Key metrics included the number of prescription fills over the first and second years, categorized weight loss outcomes, and comparison between those with and without medication interruptions.
Results
- Prevalence of interruptions:
- 72.5% experienced ≥1 treatment interruption
- 11.1% experienced multiple interruptions
- Average number of fills:
- Year 1: 8.13
- Year 2: 15.25
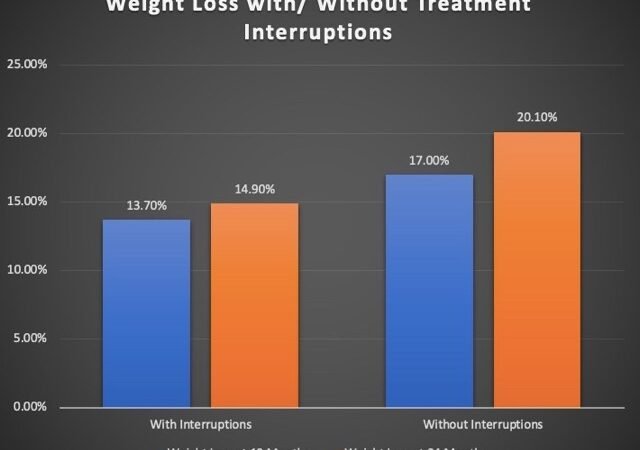
Weight Loss Outcomes:
| Treatment Status | % Weight Loss at 12 Months | % Weight Loss at 24 Months |
|---|---|---|
| With Interruption(s) | 13.7% | 14.9% |
| Without Interruptions | 17.0% | 20.1% |
Even participants who filled only 1–4 prescriptions per year achieved an average weight loss exceeding 10%, which is considered a clinically meaningful threshold for metabolic health improvement.
“These findings show that although it is frustrating for patients to lose access to medication, they can still reach their goals,” said Kaelen L. Medeiros, M.S., Director of Data and Research at Calibrate.
“Our data show that effective weight loss is possible when lifestyle changes and structured coaching are also in place.”
Clinical Implications
The study underscores several important points for clinicians:
- Weight loss is possible despite intermittent pharmacotherapy, particularly when treatment is supported by intensive lifestyle intervention.
- Integrated care models — combining pharmacologic therapy with behavioral support — may offer greater durability in weight loss outcomes, even when ideal treatment schedules are not maintained.
- Patient reassurance is essential: For those unable to maintain uninterrupted access to GLP-1 medications, clinicians can reference this data to reduce anxiety and maintain engagement.
- Lifestyle modifications retain a powerful, independent effect, and may mitigate the setbacks caused by treatment gaps.
Limitations
As a retrospective observational analysis, the study cannot confirm causality. The reliance on real-world program data, while reflecting practical scenarios, may introduce confounders not present in randomized controlled trials. Additionally, the lack of uniformity in prescription duration and dose adjustments could influence weight loss trajectories.
Future Directions
Further prospective, controlled trials are needed to:
- Quantify the minimum effective duration and frequency of GLP-1 dosing
- Identify the most protective behavioral interventions during treatment gaps
- Determine the tipping point at which treatment interruption leads to weight regain
Understanding these parameters will be critical in optimizing care for individuals with intermittent medication access.
Conclusion
The findings from the ENDO 2025 study provide reassuring evidence that clinically significant weight loss can be maintained even with GLP-1 drug interruptions. While continuous pharmacologic therapy remains the gold standard, this research highlights the importance of holistic care models that emphasize lifestyle change, behavioral coaching, and patient empowerment.
These insights offer both hope and guidance to clinicians and patients navigating the evolving landscape of obesity management amidst real-world barriers.